One in six. Let that sink in. That’s not some abstract statistic from a dusty research paper; that’s a huge chunk of the global population. And what’s affecting them? Antibiotic resistance . It’s not a sci-fi movie plot; it’s happening now, and it’s something we all need to understand. Forget the doom and gloom for a second; let’s unpack this, because understanding the problem is the first step to tackling it. So, what does this actually mean for you, me, and everyone we know?
Why Should You Care About Antibiotic Resistance? (More Than You Think!)
Okay, so antibiotic resistance is on the rise. Big deal, right? Wrong. Let’s be honest, most people only think about antibiotics when they have a nasty cough or a stubborn infection. But the overuse and misuse of these drugs have created a breeding ground for superbugs – bacteria that have evolved to resist the effects of antibiotics. A common mistake I see people make is underestimating the potential consequences. Think of it this way: antibiotics are like our superheroes against bacterial villains. But what happens when the villains develop immunity? Our superheroes become useless. Infections that were once easily treatable become life-threatening. Common surgeries become riskier. Even a simple cut could turn deadly. That’s not hyperbole; that’s the very real threat posed by the increasing prevalence of antibiotic resistant bacteria . And it’s not just a problem for individuals; it has massive implications for public health and the economy. According to the World Health Organization (WHO Fact Sheet ), antimicrobial resistance (AMR) could cost the global economy trillions of dollars annually. So, yeah, it’s kind of a big deal. Let me rephrase that for clarity, This has an effect on not only humans but animals as well, increasing the need for antibiotic stewardship .
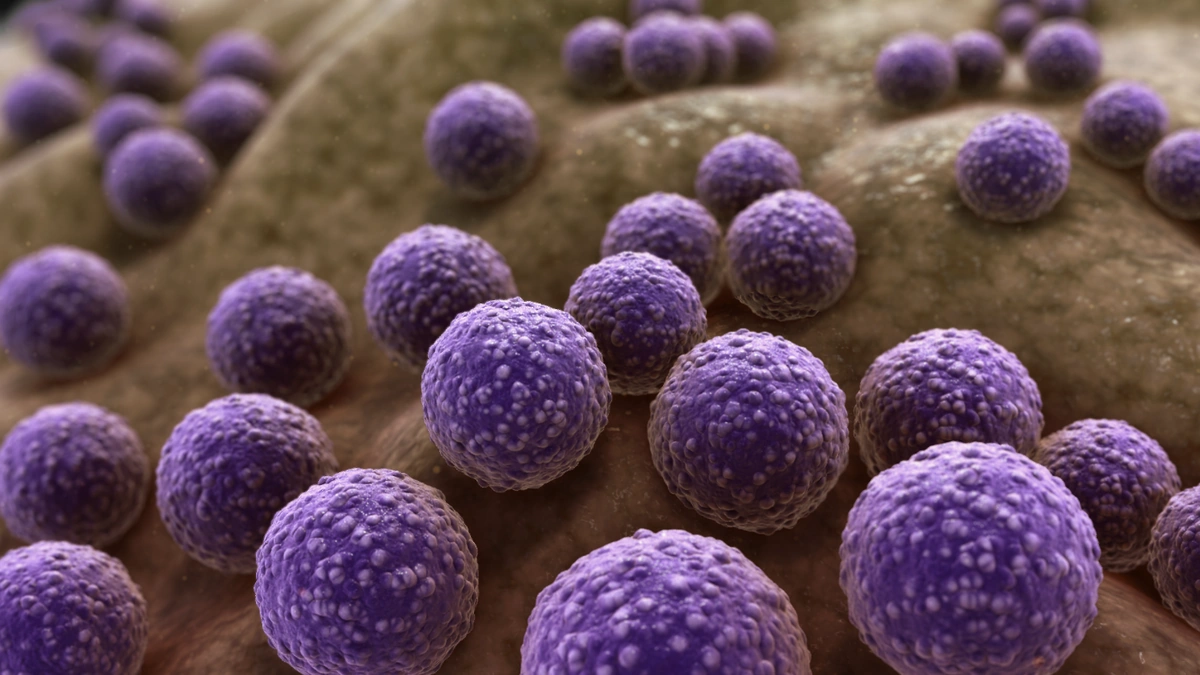
How Does Antibiotic Resistance Actually Work? (The Not-So-Simple Science)
Here’s the thing: bacteria are incredibly adaptable. They can evolve much faster than we can develop new antibiotics. When we use antibiotics, we’re essentially creating a selective pressure that favors resistant bacteria. The non-resistant bacteria get wiped out, while the resistant ones survive and multiply, passing on their resistance genes to future generations. It’s like a Darwinian arms race playing out in our bodies. Now, bacteria can also share these resistance genes with each other through a process called horizontal gene transfer. This means that even bacteria that aren’t directly exposed to antibiotics can become resistant. What fascinates me is how quickly bacteria can adapt to new threats. It’s a constant evolutionary battle, and we need to be smarter about how we use antibiotics if we want to stay ahead. This includes understanding the role of genetic mutations and how they contribute to resistance.
Practical Steps You Can Take to Fight Antibiotic Resistance (Starting Today!)
Okay, so the situation is serious, but it’s not hopeless. There are things we can all do to help slow down the spread of antibiotic resistant infections . First and foremost, only take antibiotics when they’re truly necessary, and always follow your doctor’s instructions. Don’t pressure your doctor to prescribe antibiotics if they don’t think you need them. Remember, antibiotics only work against bacterial infections, not viral infections like the common cold or flu. A common mistake I see people make is stopping their antibiotic course as soon as they start feeling better. It is important to finish the entire course of antibiotics, even if you feel better before it’s done. This helps to ensure that all the bacteria are killed and reduces the risk of resistance developing. Another thing is to practice good hygiene. Wash your hands frequently with soap and water, especially after using the bathroom and before eating. This helps prevent the spread of bacteria, including resistant ones. We must also push for better infection prevention and control measures in hospitals and other healthcare settings. We can checkmeasles cases in the U.S.for more health related news.
The Role of Agriculture in Antibiotic Resistance (It’s Bigger Than You Think)
Here’s where things get even more interesting. A significant amount of antibiotics are used in agriculture, primarily to promote growth and prevent disease in livestock. This overuse of antibiotics in animals is a major contributor to the rise of antibiotic resistant bacteria in agriculture . The resistant bacteria can then spread to humans through the food chain or through direct contact with animals. The one thing you absolutely must realize is that this is a global problem. The use of antibiotics in agriculture varies widely from country to country, but it’s a concern everywhere. There is a growing movement towards reducing antibiotic use in agriculture, with some countries implementing stricter regulations. But more needs to be done to ensure that antibiotics are used responsibly in both human and animal medicine. This includes investing in research to develop alternative strategies for disease prevention and growth promotion in livestock. For more information checkMMR vaccine single dose.
Looking Ahead | Innovation and Hope in the Fight Against Resistance
So, where do we go from here? The fight against antibiotic resistance is an ongoing one, but there’s reason to be hopeful. Scientists are working on developing new antibiotics, as well as alternative therapies that can help fight bacterial infections without contributing to resistance. These include things like phage therapy, which uses viruses to kill bacteria, and immunotherapy, which boosts the body’s own immune system to fight infection. We must continue investing in research and development to find new ways to combat antibiotic resistance. And we need to promote responsible antibiotic use through education and awareness campaigns. The future of medicine depends on it. It’s also important to note that rapid diagnostic tests are a key tool in combating antibiotic resistance. They allow doctors to quickly identify the cause of an infection and prescribe the right antibiotic, avoiding unnecessary use. Let’s be honest, the challenge is huge, but with a combination of innovation, responsible use, and global cooperation, we can turn the tide on antibiotic resistance.
FAQ | Antibiotic Resistance Explained
Frequently Asked Questions
What exactly is antibiotic resistance?
Antibiotic resistance happens when bacteria change in a way that reduces or eliminates the effectiveness of antibiotics designed to cure infections. The bacteria survive and continue to multiply, causing more harm.
How does antibiotic resistance spread?
It spreads through various ways, including: direct contact with people, animals, or the environment; through the food chain; and via international travel.
Can I prevent antibiotic resistance myself?
Yes! Take antibiotics only when prescribed, complete the full course, practice good hygiene (wash hands!), and get vaccinated.
Is antibiotic resistance a problem only in hospitals?
No, it’s a community-wide issue. While hospitals can be hotspots, resistant bacteria can be found anywhere – homes, schools, farms, etc.
What’s the difference between antibiotic and antimicrobial resistance?
Antibiotics target bacteria, while antimicrobials target a broader range of microbes, including bacteria, viruses, fungi, and parasites. Antimicrobial resistance is the broader term.
Where can I learn more about antibiotic resistance?
Check out the CDC (Centers for Disease Control and Prevention) and WHO (World Health Organization) websites for reliable information.
The fight against antibiotic resistance is a marathon, not a sprint. It requires a sustained effort from all of us individuals, healthcare professionals, policymakers, and researchers to protect the effectiveness of these life-saving drugs for future generations. So, let’s start today. Let’s be the change that ensures a healthier tomorrow for everyone.