Okay, let’s be real. You’ve probably seen headlines about antibiotic resistance before. Maybe you even skimmed past them. But this isn’t just another news blip – it’s a slow-motion crisis unfolding right before our eyes, and the latest WHO report is flashing red, especially for us in India. So, why should you care? That’s what we’re diving into. Not just the scary numbers, but the real-life implications and what, if anything, can be done.
The Silent Pandemic | Why Antibiotic Resistance Matters
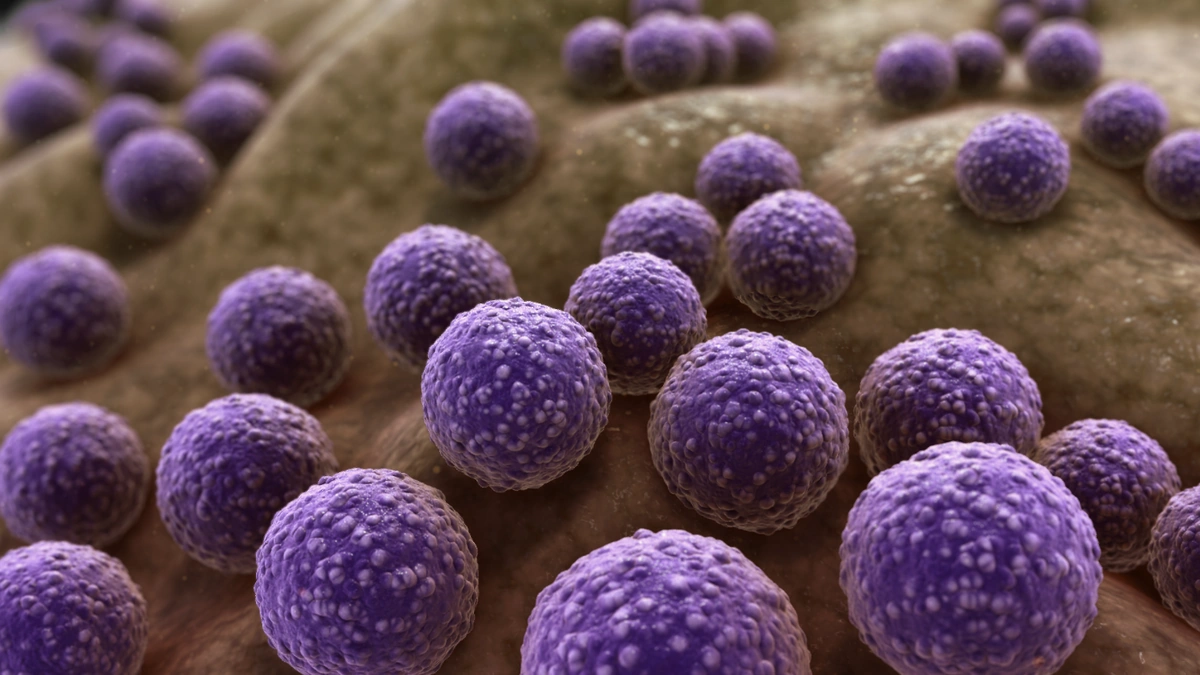
Here’s the thing: antibiotics have been a cornerstone of modern medicine. They’ve saved countless lives from bacterial infections. But over time, bacteria – those tiny, relentless organisms – have learned to outsmart these drugs. They develop resistance. Think of it like this: it’s an evolutionary arms race, and the bacteria are currently winning. The WHO report simply confirms what many experts have been warning about for years: this resistance is spreading faster than we can develop new drugs to combat it.
And why does it matter so much? Because simple infections can become deadly. Surgeries become riskier. The cost of healthcare skyrockets. It’s not just about a longer hospital stay; it’s about whether or not treatments work at all. Globally, the situation is alarming, but India’s high population density, sanitation challenges, and widespread over-the-counter availability of antibiotics make it a particularly vulnerable hotspot. That is a lethal combination. We need to think about antimicrobial resistance surveillance to prevent further spread.
India’s Unique Challenges | A Perfect Storm for Resistance
Let’s be honest, we’re not exactly known for our strict adherence to medical protocols when it comes to antibiotics. How many times have you popped an antibiotic for a minor cold, or stopped the course midway because you felt better? I’ve been guilty of it myself. That ease of access is a major problem. Many pharmacies in India will happily dispense antibiotics without a prescription – a practice that fuels misuse and, consequently, antibiotic resistance in India .
Beyond that, sanitation and hygiene play a significant role. Poor sanitation facilities contribute to the spread of resistant bacteria. And the overuse of antibiotics in agriculture – to promote growth in livestock – further exacerbates the problem, leading to multi-drug resistance in bacteria that can then jump to humans. It’s a complex web of interconnected factors that demands a multifaceted approach.
What Can Be Done? A Call to Action
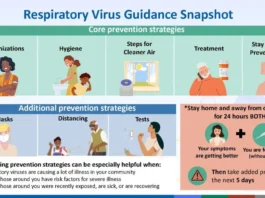
So, are we doomed? Absolutely not. But it requires urgent and coordinated action on multiple fronts. Public health campaigns are crucial to educate people about the responsible use of antibiotics. We need to drive awareness about antimicrobial stewardship programs . Stricter regulations are needed to curb over-the-counter sales and ensure proper prescriptions. Investment in research and development of new antibiotics is essential, though notoriously underfunded. And improved sanitation and hygiene practices are non-negotiable.
But it’s not just about government policies and scientific breakthroughs. Each of us has a role to play. Think twice before demanding antibiotics from your doctor for a viral infection. Complete the full course of medication, even if you feel better. Practice good hygiene – wash your hands regularly. These small steps, multiplied across a billion people, can make a huge difference. Furthermore, the proper use of diagnostic tests can help identify the right treatments and reduce the misuse of antibiotics.
The Economic Burden | A Ticking Time Bomb
Beyond the immediate health consequences, antibiotic resistance poses a significant economic threat. As infections become harder to treat, healthcare costs will inevitably rise. Longer hospital stays, more expensive medications, and reduced productivity all contribute to a growing economic burden. The World Bank estimates that antimicrobial resistance could cost the global economy trillions of dollars by 2050. This isn’t just a health issue; it’s an economic one too, and India, with its large population and developing economy, stands to lose significantly if we don’t act decisively.
According to the World Health Organization (WHO) , antimicrobial resistance (AMR) occurs when bacteria, viruses, fungi and parasites change over time and no longer respond to medicines making infections harder to treat and increasing the risk of disease spread, severe illness and death.
Beyond Treatment | Prevention is Key
The focus shouldn’t solely be on treating resistant infections; preventing them in the first place is crucial. Vaccination programs play a vital role in reducing the incidence of bacterial infections, thereby lessening the need for antibiotics. Promoting breastfeeding, ensuring safe food handling practices, and controlling infections in hospitals are all essential preventive measures. A shift towards preventive healthcare is not just desirable, it’s a necessity in the fight against antibiotic resistance.
The issue of antibiotic stewardship is critical to preventing the spread of resistance. We need to shift the mindset from antibiotics as a first resort to a last resort. Prudent use, guided by accurate diagnostics and responsible prescribing, is the only way to preserve the effectiveness of these life-saving drugs. Measles vaccinations are an excellent way to prevent certain bacterial infections.
So, yeah, the WHO report paints a grim picture. But it’s not a prophecy of doom – it’s a wake-up call. A call to action for governments, healthcare professionals, and each and every one of us. Because the fight against antibiotic resistance isn’t some abstract, far-off battle. It’s happening right here, right now, and the future of healthcare in India depends on how we respond.
FAQ | Antibiotic Resistance in India
What exactly is antibiotic resistance?
It’s when bacteria evolve to become resistant to antibiotics, making infections harder (or impossible) to treat.
Why is India so affected by this?
Over-the-counter availability of antibiotics, poor sanitation, and overuse in agriculture are key factors.
What can I do to help prevent it?
Don’t demand antibiotics for viral infections, complete the full course, and practice good hygiene.
Are there any new antibiotics being developed?
Research is ongoing, but the pace is slow, and resistance is developing faster than new drugs.
Where can I find more information?
Consult your doctor or check the WHO website for reliable resources.
Is organ transplant affected by antibiotic resistance?
Yes, the risk of infection is high in people undergoing organ transplant.